
The patient was suspected of having an intracranial bleed; agitated with abnormal extensor posturing and actively vomiting. They clearly needed an RSI (rapid sequence induction of anaesthesia and tracheal intubation), but despite the apparently low Glasgow Coma Scale (GCS) score every time a face mask was applied they twisted away from it, becoming even more agitated and thwarting our best attempts to provide effective pre-oxygenation. Also, it was hard to keep the monitoring leads on, and the two points of intravenous access were threatening to become dislodged.
Every experienced emergency airway practitioner has met this patient, and wondered what to do for the best. Sometimes they will tolerate a simple reservoir mask with high flow oxygen, and sometimes they won’t. Sedation can facilitate pre-oxygenation, but only if you haven’t given so much that the patient is no longer breathing effectively, and sedation also obtunds airway reflexes so if the patient does vomit there is an increased risk of pulmonary aspiration.
In 2011 Scott Weingart coined the term “delayed sequence intubation” to describe the administration of ketamine (1mg/kg as a slow IV push) to agitated patients in order to facilitate effective preoxygenation. This gave a name to a practice that had been in use for decades, but which was rarely taught or discussed. 1mg/kg of ketamine can be a significant dose in critically ill or injured patients, and even given slowly IV there is a very real risk of respiratory depression, vomiting, aspiration and laryngospasm. There are alternative approaches, and these are often discussed during the high-fidelity simulations that are used as the mainstay of teaching on the UK Training in Emergency Airway Management (TEAM) Course.
Firstly, in any emergency situation you should always use drugs and techniques with which you are familiar, and with which you have gained experience in less stressful situations, under supervision. Ketamine is increasingly familiar to emergency airway practitioners, and is fast becoming the induction drug of choice in critical illness and injury. However it makes little sense to give ketamine if that is not your intended induction drug; the risks of polypharmacy and drug error are real, and I would always recommend either a small and carefully titrated dose of the drug you are planning to use for induction, or a benzodiazepine with which you are very familiar.
Small doses, titrated to effect, are often sufficient in this situation, and minimise risk. I commonly find that 0.25mg/kg of ketamine (repeated if necessary) is effective in preparing the patient for RSI. You can always put more drug into a patient, but once it’s in a vein you can’t get it back out again! It is therefore essential to be fully prepared for any eventuality, including respiratory arrest and vomiting.
The other side to this problem is the question of how much pre-oxygenation is enough pre-oxygenation. On the assumption that “8 vital capacity breaths over one minute of 100% O2 via a tightly fitting face-mask” isn’t something that your patient will be persuaded to engage with, this leaves the option of trying to get an agitated individual to breathe 100% oxygen at normal tidal volumes for three minutes. Three minutes is achievable; the challenge is 100% oxygen when the tighter and more effective the seal the more likely it is that an agitated and confused patient will object. This is further compounded by the resistance to breathing that is inherent in a “bag-valve-mask”, which is the most common device used for pre-oxygenation in a patient requiring emergency RSI outside the operating theatre. Ten years ago, I was involved in some research with Rob Stafford and Jerry Nolan which showed that a Mapleson C breathing system was superior to a self-inflating bag, for both pre-oxygenation and user comfort in healthy volunteers. This translates well into clinical practice, and it is well worth considering a Mapleson C system if one is available and you are trained to use it since it offers no resistance to spontaneous ventilation and is better tolerated by an agitated patient.
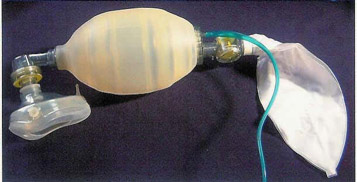

A word of caution though… Mapleson C systems can deliver a hypoxic mixture if the fresh gas flow fails, and they don’t work in the absence of an oxygen supply. Therefore you should never, ever go anywhere with a critically ill patient without a self-inflating bag-valve-mask system; if the worst happens this is the device that will allow you to continue to ventilate a patient on air, and it really beats blowing down a tracheal tube!
For very agitated patients a simple facemask with a reservoir bag remains a possibility, and is sometimes very well tolerated by agitated patients, particularly when turned up to a very high oxygen flow, because it avoids the feeling of claustrophobia and suffocation that can be associated with a tight-fitting face mask. The problem, however, is that a reservoir mask simply isn’t as good as a tight-fitting facemask because the oxygen supply into the mask (conventionally set at 15 l/min) can’t keep up with the patient’s peak inspiratory flow (which often exceeds 60 l/min). The entrainment of air around the mask therefore becomes inevitable, even in the presence of a well-functioning reservoir bag (and most reservoir bags are not well functioning; they should be fully inflated before application and visibly collapse with every breath; a very rare sight indeed). This may be assisted by increasing the oxygen flow into the mask substantially (to 30 l/min or more), and by adding oxygenation through nasal canulae, though the effectiveness of this latter modification is contested, and has achieved mixed results in the research published to date.
So, back to our patient. Options include a simple reservoir mask with the highest oxygen flow achievable, and possibly additional oxygenation by nasal canulae, if the patient will accept this, but bear in mind that the degree of oxygenation achieved will almost certainly be sub-optimal. Alternatively, cautious titrated sedation may allow effective preparation and pre-oxygenation with a tight-fitting facemask connected to a bag-valve-mask or Mapleson C breathing system. The latter remains the approach of choice, if you have the oxygen supply and the skill to use it.
References
- Weingart SD. Preoxygenation, Reoxygenation, and Delayed Sequence Intubation in the Emergency Department. J Emerg Med 2011;40(6):661-667.
http://tdh.org.nz/assets/ED/2012/JanFeb/preoxreoxarticle.pdf - Tanoubi I, Drolet P, Donati F. Optimizing pre-oxygenation in adults. Can J Anesth2009;56:449–466.
https://link.springer.com/article/10.1007/s12630-009-9084-z - Stafford R, Benger J, Nolan J. Self-inflating bag or Mapleson C breathing system for emergency pre-oxygenation? Emerg Med J2008;25:153-155.
http://eprints.uwe.ac.uk/5227/1/Download.pdf - Groombridge C, Chin CW, Hanrahan B, Holdgate A.Assessment of Common Preoxygenation Strategies Outside of the Operating Room Environment. Acad Emerg Med2016;23(3):342-6. doi: 10.1111/acem.12889.
https://onlinelibrary.wiley.com/doi/pdf/10.1111/acem.12889 - Hayes-Bradley C, Lewis A, Burns B, Miller M. Efficacy of Nasal Cannula Oxygen as a Preoxygenation Adjunct in Emergency Airway Management. Ann Emerg Med2016;68(2):174-80.
http://www.psnetwork.org/wp-content/uploads/2017/04/Scott-NP1.pdf

Leave a reply