‘Patients with GCS scores of 8 or less require prompt intubation.’
ATLS; 9thedition
The mantra of GCS 8, intubate has pervaded teaching for those involved in the management of patients with a reduced GCS (Glasgow Coma Scale).
On reflection it would seem slightly odd that the gaining or loss of a single point on the Glasgow Coma Scale could simply account for a change in the decision as to whether a patient would benefit from intubation and ventilation. So should the patient with a GCS of 9 be best managed without a definitive airway, but when that slips to 8 we should reach for the portex®?
To answer this lets have a bit more of a think about the Glasgow Coma Scale. The scale was initially described in 1974 in the Lancet by Teasdale as a way to explicitly describe the level of consciousness that a patient held following an acute brain trauma and plot the changes in consciousness as they occurred.
As we know the GCS is made up of 3 parts, eyes, verbal and motor, each holding an individual score which when added together will lie somewhere from 15 (fully conscious) to 3 (totally unresponsive). The scale was adopted by health care professionals due to its simplicity of use, and as a scale in which progression or resolution of symptoms could easily be tracked.
The Glasgow Coma Scale and it’s constituents
| Score | Eye opening | Verbal | Motor |
| 6 | Obeys commands | ||
| 5 | Patient orientated | Localises to pain | |
| 4 | Spontaneously | Patient confused | Withdraws from pain |
| 3 | To voice | Inappropriate words | Flexion to pain |
| 2 | To pain | Incomprehensible sounds | Extensor response to pain |
| 1 | No eye opening | None | None |
The first iteration of the Advanced Trauma Life Support course recommended utilisation of GCS for all trauma patients, with the approach of a patient with a score of 8 or less requiring intubation.
This approach to airway management plans has also crept into the non-trauma cohort as a significant part of the decision making process regarding ongoing management of the airway. But should it, and in fact does this statement hold true in the trauma cohort?
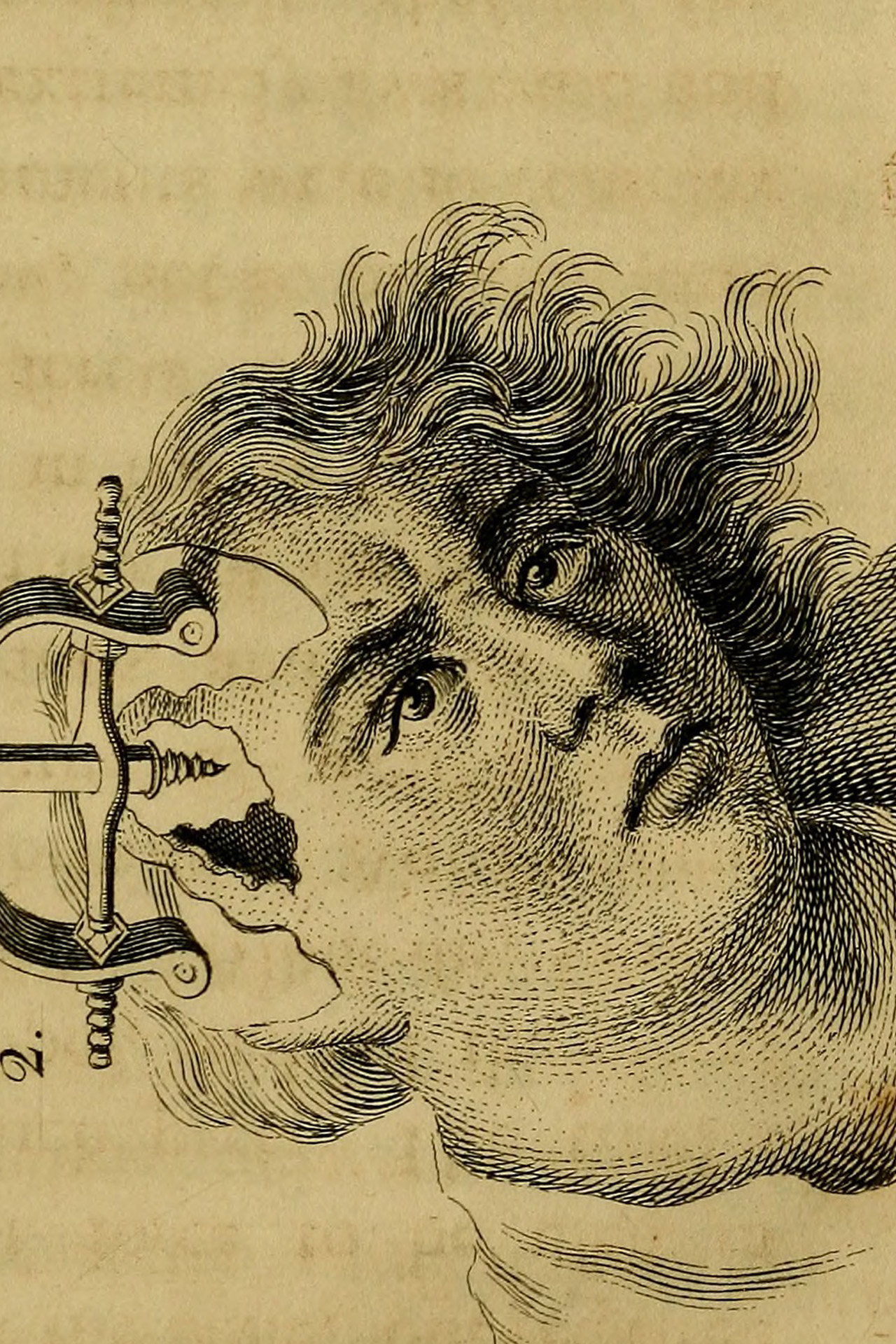
In 2011 Green published regarding the weaknesses of the GCS scale in an article entitled ‘Cheerio, Laddie. Bidding Farewell to the Glasgow Coma Scale.’ In this he highlighted the previously documented low interrater reliability, with some studies showing different assessments of GCS agreeing in approximately 1 in 3 patients, therefore suggesting a need to approach the GCS with a degree of error margin. This inaccuracy of GCS extends to both those reviewing the patients in the emergency setting and those carrying scalpels and drills considering definitive surgical procedures.
A patient can gain a GCS score with multiple permutations of its constituents, holding very different significance. Healey reported the associated mortality of the 3 different make-ups of a GCS 4 lay between 19-48%, where utilisation of the motor component of the score alone showed better correlation with survival.
A decreased conscious level in the acute setting is not, by any means, most frequently due to trauma, and includes other frequent precipitants such as intoxication, infection and intracerebral catastrophes.
In a small ED study Duncan described a prospective cohort of patients with decreased GCS scores (ranging from 3-14) as a result of drug or alcohol intoxication. Only one required intubation and none of the patients with a GCS of 8 or less required intubation, or aspirated.
So how likely are you to lose your gag reflex if your GCS drops? A study from Rotherhay showed, as you might expect, that gag and cough reflexes decrease with a decreasing GCS in patients requiring critical care. But they didn’t show a sudden drop at a GCS of 8. In those with a GCS of 9-14 they found absent reflexes in 37% and in those with a GCS of 8 or less, 63% had an absent gag reflex but, perhaps most surprisingly, in those with a full GCS score of 15, 22% hadn’t got a gag reflex!
Sadly there is no RCT showing the risk/benefit profile of intubation in low GCS patients versus a conservative approach and so for the meantime we will have to work with the evidence that we have to hand. So how should we assess the need for intubation in patients with a decrease GCS?
The TEAM Course teaches the following indications for intubation
- The apnoeic patient
- Patient with an obstructed or partially obstructed airway where basic care is ineffective
- Patient requiring invasive respiratory support for oxygenation or ventilator failure
- Patient in whom basic airway care is effective, but whose predicted clinical course includes a high probability of airway obstruction, aspiration or ventilator failure.
It is in this final cohort of patients that the patient with the decreased GCS lies. In these patients a systematic review of the risks vs benefits of intubation and ventilation needs to occur. In the meantime we are left to make a pragmatic evaluation of the risk of a difficult or complicated intubation against the risk of airway compromise in the context of the patient’s likely clinical course; is this a likely short lived toxidrome or are they likely to improve in the next short period?
So, in summary; don’t ignore that GCS but maybe beware of decision making purely on that magic number 8…
Simon Laing
References
Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013;74(5):1363-6.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81-4.

Leave a reply